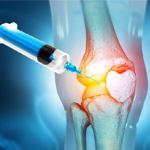
Platelet-rich plasma (PRP) therapy has gained significant attention and application in orthopedics over recent years. This innovative treatment involves injecting a concentrated form of a patient’s own blood, rich in platelets, into damaged tissues or joints to promote healing and regeneration. In orthopedics, PRP has been utilized for various conditions, including tendon injuries, osteoarthritis, ligament injuries, and muscle strains.
The premise behind PRP therapy lies in the regenerative properties of platelets. Platelets contain numerous growth factors and cytokines that play crucial roles in the healing process. When injected into injured tissues, PRP can stimulate tissue repair mechanisms, enhance collagen production, and promote angiogenesis, which is the formation of new blood vessels. These effects contribute to accelerated healing and improved functional outcomes for patients with orthopedic injuries.
One of the significant advantages of PRP therapy in orthopedics is its minimally invasive nature. Unlike surgical interventions, PRP injections can often be performed in an outpatient setting, reducing the risk of complications and shortening recovery times. Additionally, because PRP is derived from the patient’s own blood, the risk of allergic reactions or rejection is minimal, making it a safe treatment option for many individuals.
In clinical practice, PRP therapy has been utilized across various orthopedic subspecialties. For example, in sports medicine, PRP injections have been employed to treat common injuries such as tendonitis, tennis elbow, and rotator cuff tears. In orthopedic surgery, PRP may be used as an adjunctive treatment to promote tissue healing following procedures such as ligament reconstructions or joint replacements. PRP has shown promising results in the management of degenerative joint conditions like osteoarthritis, where it can help alleviate pain and improve joint function.
While the use of PRP in orthopedics holds considerable potential, ongoing research is needed to further elucidate its optimal indications, dosing protocols, and long-term efficacy. Additionally, challenges such as standardization of PRP preparation methods and variability in patient responses underscore the importance of continued investigation and refinement of this treatment modality. Nonetheless, with its ability to harness the body’s natural healing mechanisms, PRP therapy remains a valuable tool in the orthopedic armamentarium, offering patients an alternative approach to manage a wide range of musculoskeletal conditions
For further information, consult the Santa Barbara Bone and Joint Clinic.